Tissue perfusion pressure enables continuous hemodynamic evaluation and risk prediction in the intensive care unit, according to new research paper
Mindy Blodgett | IMES
Anand Chandrasekhar, who is doing post-doctoral work at the Institute for Medical Engineering and Science (IMES), is one of the lead authors of a paper on exciting new research creating a novel method for monitoring patients in the intensive care unit. This research is aimed at optimizing therapies for conditions such as circulatory shock, heart failure, and others. The main focus of the research approach was to devise a way to measure a fundamental circulation property referred to as “critical closing pressure”.
According to Chandrasekhar, “individuals afflicted with heart failure or circulatory shock necessitate vigilant monitoring and intensive care.”
“A paramount objective of their treatment revolves around maintaining sufficient blood pressure levels to avert harm to vital organs,” Chandrasekhar says. “This study introduced an innovative approach to monitoring ICU patients, holding the potential for enhanced management of blood pressure and heart function. Consequently, this advancement may lead to a reduced risk of mortality and other adverse outcomes.”
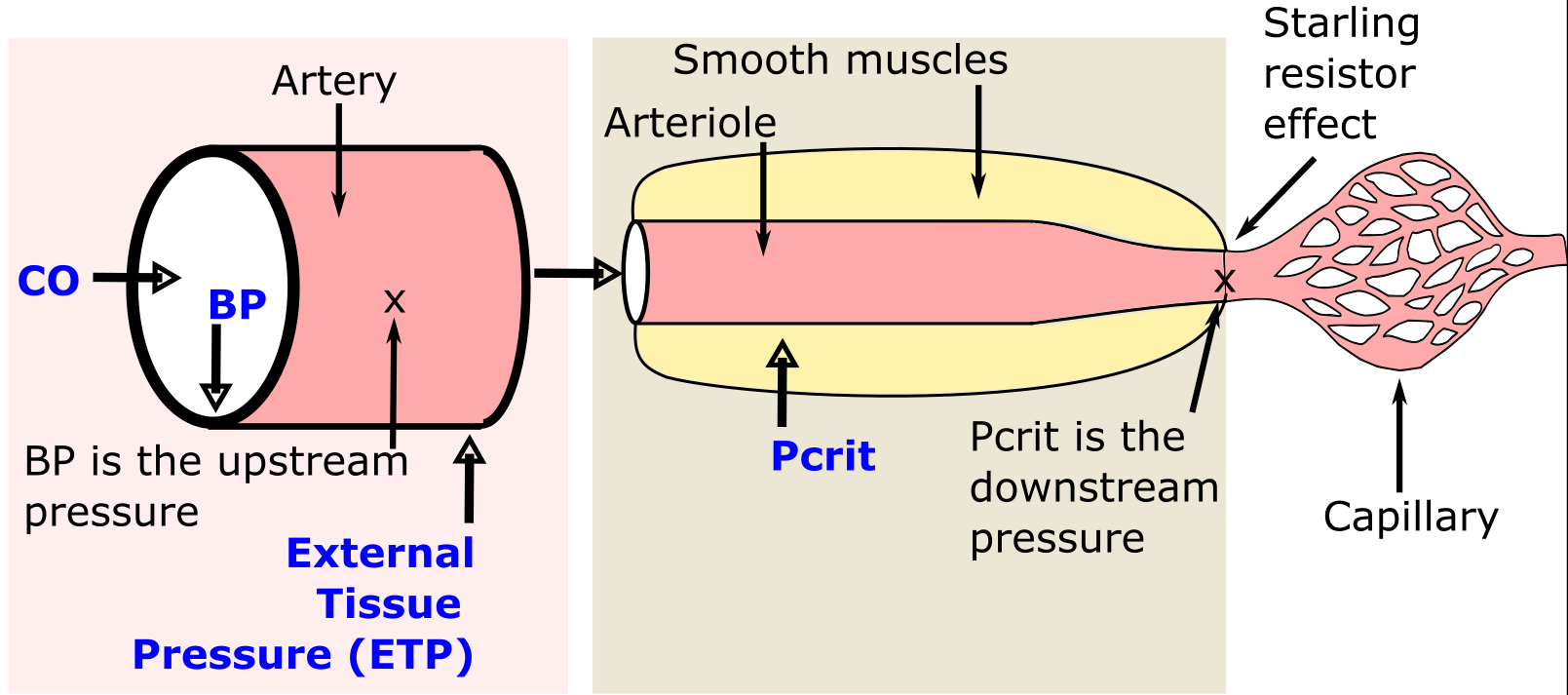
Charles Sodini, LeBel Professor of Electrical Engineering, MIT, a core faculty member at IMES, and a co-author, said of the importance of the new research: “Tissue Perfusion Pressure (TPP) is a new metric that can be an additional tool, along with other macroscopic hemodynamic parameters such as Mean Arterial Pressure (MAP) and Cardiac Output (CO), that clinicians can use in the ICU for monitoring a patient to adjust treatment for circulatory shock and heart failure.”
Aaron D. Aguirre, MD, PhD, who is a 2008 Medical Engineering and Medical Physics (MEMP) PhD graduate of the Harvard-MIT Program in Health Sciences and Technology (HST), as well as an HST MD alum, is also a co-author (IMES is HST’s home at MIT).
“In this work, we developed a new approach to measuring a fundamental property of the human circulation called the critical closing pressure, which is the arterial blood pressure at which blood flow stops and the vessels collapse,” says Aguirre, a cardiologist and critical care doctor at Massachusetts General Hospital. “We use this new measurement to calculate a parameter that we call (the TPP), and we then showed that TPP correlates with many important outcomes, including mortality, in patients in a cardiac intensive care unit. We believe that TPP may offer a new metric for optimizing therapies in patients in the intensive care unit.”
Chandrasekhar says that next steps for the research include pursuing further investigations to understand how tissue perfusion pressure varies with important therapies. “Most importantly, we will design clinical trials aimed at demonstrating that the new measurement can guide management and improve outcomes in critically ill patients,” Chandrasekhar says.
Read more about the research in the paper recently published in Nature Medicine.
